Views: 222 Author: Lake Publish Time: 2026-02-15 Origin: Site








Content Menu
● Understanding the Laryngoscope Handle: Types and Infection Risks
>> Classification of Laryngoscope Handles
● General Principles and Pre-Cleaning Protocols
>> Point-of-Care Immediate Cleaning
>> The Critical Importance of Manufacturer Instructions
● Step-by-Step Cleaning and Disinfection for Reusable Metal Handles
>> Phase 1: Disassembly and Preparation
>> Phase 2: Manual Cleaning—The Non-Negotiable Foundation
>> Phase 3: Disinfection or Sterilization
>> Phase 4: Rinsing, Drying, Reassembly, and Storage
● Special Considerations for Video Laryngoscope Handles
● Common Errors and How to Avoid Them
● The Role of Single-Use Alternatives and Protective Barriers
● Frequently Asked Questions (FAQs)
>> 1. Can I clean a laryngoscope handle by simply wiping it with an alcohol swab?
>> 2. How often should the batteries in a reusable laryngoscope handle be changed?
>> 3. Is it acceptable to store the laryngoscope handle with the blade attached?
>> 4. What should I do if a laryngoscope handle is damaged (cracked, corroded, broken latch)?
>> 5. What is the advantage of using a disposable plastic sheath over a laryngoscope handle?
In the intricate practice of airway management, the laryngoscope stands as an indispensable tool for visualization and intubation. While considerable attention is rightfully devoted to cleaning the laryngoscope blade—the component that directly contacts mucous membranes—the laryngoscope handle demands equally rigorous attention in infection prevention protocols. The handle, frequently touched by clinicians' hands during procedures and often exposed to droplet contamination from the patient's airway, can become a significant reservoir for pathogens, posing a genuine risk of cross-contamination between patients. As a company specializing in medical visualization and OEM manufacturing of precision devices like endoscopes and bronchoscopy workstations, we understand that the durability and cleanability of every component, including the laryngoscope handle, are fundamental design considerations. This comprehensive guide provides a detailed, evidence-based protocol for properly cleaning and disinfecting laryngoscope handles, ensuring both patient safety and device longevity.

Before establishing cleaning protocols, it is essential to understand the different types of laryngoscope handles, as each requires specific reprocessing approaches .
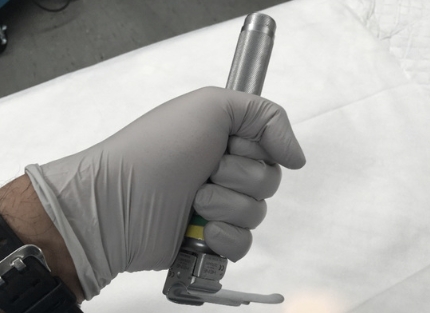
Reusable Metal Handles: The traditional and most common type, typically constructed from stainless steel or chrome-plated brass. These are durable, designed for repeated use, and house the batteries that power the light source. They must undergo rigorous reprocessing between each patient use.
Disposable Handles: Made from plastic materials, these are intended for single use and are discarded after a procedure. Often pre-assembled with a blade, they eliminate reprocessing requirements but still demand proper disposal as medical waste.
Video Laryngoscope Handles: Used with advanced video laryngoscope systems, these contain electronic components, screens, and charging ports. They require very specific cleaning procedures to prevent liquid ingress and damage to sensitive electronics.
Rechargeable System Handles: Proprietary handles designed for specific video laryngoscope systems, often with integrated batteries and complex electronic interfaces.
Historically, the laryngoscope handle was considered a non-critical item that contacts only intact skin . However, contemporary infection control understanding classifies both the laryngoscope blade and handle as semi-critical items requiring at least high-level disinfection (HLD) or sterilization when possible . This reclassification stems from compelling evidence:
- The laryngoscope handle is frequently contaminated during use, as the blade often touches the handle and contaminates it with blood or secretions .
- Pathogens can survive on handle surfaces for extended periods, creating reservoirs for cross-contamination.
- A serious patient infection and death has been documented in association with a contaminated laryngoscope handle, highlighting the critical nature of proper reprocessing .
This evidence underscores that thorough cleaning of laryngoscope handles is not merely a recommendation but an absolute necessity for patient safety.
Always treat every laryngoscope handle as potentially contaminated. Personnel handling soiled devices must wear appropriate personal protective equipment (PPE), including medical gloves and a fluid-resistant gown .
The reprocessing cycle begins immediately after use, before the device is transported to the central sterile supply department (CSSD). At the bedside or procedure area, the laryngoscope handle should be wiped with a facility-approved disinfectant wipe to remove gross contamination . This immediate action prevents organic material from drying and hardening on the handle surface, which significantly complicates subsequent cleaning steps.
During this bedside cleaning, particular attention should be paid to the blade locking mechanism, textured grip areas, and any crevices where debris may accumulate . Following this initial wipe, the laryngoscope handle should be carefully separated from the blade and placed in a designated, labeled, leak-proof container for transport to the reprocessing area.
The single most important step in any reprocessing protocol is consulting the manufacturer's Instructions for Use (IFU) for the specific laryngoscope handle model . The IFU provides the only approved methods for cleaning and disinfection that will not void warranties or damage the device. Different handles have different material compositions, seals, and electronic components that dictate compatible cleaning agents and methods. The following steps represent a general framework, but must always be validated against the specific device's IFU.
Proper disassembly is the foundation of effective cleaning :
1. Separate Components: Ensure the laryngoscope blade is completely detached from the handle. These components are typically reprocessed separately.
2. Remove Bulb Housing: For handles with removable bulb housings or bottom caps, open these according to the IFU to access internal components.
3. Battery Removal: Always remove the batteries before any wet cleaning process . Cleaning a laryngoscope handle with batteries inside can lead to corrosion, electrical failure, and inadequate disinfection of internal contacts. Batteries should be inspected for leakage and discarded if compromised.
4. Initial Inspection: Visually examine the disassembled handle for visible damage, cracks, corrosion, or wear that might compromise function or cleanability . Damaged handles should be removed from service immediately.
Effective disinfection is impossible without prior thorough cleaning to remove organic material (blood, saliva, secretions) . This phase requires meticulous attention.
Preparation of Cleaning Solution:
- Fill a clean basin with warm water and a compatible, neutral pH enzymatic detergent at the concentration specified by the detergent manufacturer.
- The water should be lukewarm (typically below 45°C/113°F) to prevent protein coagulation .
Mechanical Cleaning Process:
1. Pre-Rinse: Rinse the handle under lukewarm running water to remove loose debris.
2. Immersion and Brushing:
- Fully immerse the laryngoscope handle in the enzymatic detergent solution .
- Allow it to soak for the time specified by the detergent manufacturer (typically 5-10 minutes) to loosen adherent debris.
- Using soft-bristled brushes specifically designed for medical instrument cleaning, thoroughly scrub all external surfaces of the handle.
- Pay special attention to crevices, the blade locking mechanism, and any textured grip areas where organic material may accumulate .
- Use a small, round plastic brush to clean difficult-to-access places, brushing at least five times .
- For electrical contacts and the battery compartment interior, use cotton swabs or small brushes moistened with detergent to clean gently without damaging sensitive components .
3. Rinsing:
- Thoroughly rinse the laryngoscope handle under clean, running water to remove all detergent residue .
- Perform a final rinse with demineralized or distilled water to prevent mineral deposits and spotting .
- Residual detergent can inactivate subsequent disinfectants, making this step critical.
4. Drying:
- After rinsing, air-dry the handle completely on a clean, lint-free towel in a low-dust environment .
- Use compressed air or a dedicated air duster to remove moisture from the battery compartment and electrical contacts .
- Ensure the handle is bone dry before proceeding to disinfection or reassembly.
Following meticulous cleaning, the laryngoscope handle must undergo either high-level disinfection or sterilization, depending on the device's design and institutional policy .
High-Level Disinfection (HLD): This is the standard for most reusable laryngoscope handles .
- Immersion Method (if IFU permits): Submerge the handle in an EPA-registered high-level disinfectant (such as glutaraldehyde, ortho-phthalaldehyde, or peracetic acid) for the exact contact time specified by both the disinfectant manufacturer and the laryngoscope IFU . Avoid air pockets that could shield surfaces .
- Wipe Method (for non-immersible handles): If immersion is not permitted (common for most standard handles due to battery contact risks), use a cloth saturated with an approved disinfectant to thoroughly wet all surfaces of the handle and maintain wet contact for the required time (e.g., 3-10 minutes, depending on the agent) . Important: Wiping alone does not achieve high-level disinfection or sterilization . For true HLD, immersion or a low-temperature sterilization method is required.
Sterilization: Preferred when possible, but not always feasible for all handle types .
- Low-Temperature Sterilization: Some laryngoscope handles are compatible with hydrogen peroxide gas plasma (e.g., STERRAD®) or ethylene oxide (EtO) sterilization . This is ideal but requires specific packaging and cycle parameters.
- Autoclaving (Steam Sterilization): Most standard laryngoscope handles with plastic components, seals, or electronics are NOT autoclavable . Autoclaving will destroy them. Only handles specifically labeled as "autoclavable" can undergo this process, and even then, batteries must be removed first . Flash autoclaving is never permitted .
Automated Washer-Disinfectors: For facilities with appropriate equipment, automated washer-disinfectors can provide standardized reprocessing . When using these systems:
- Load handle shells with their large openings pointing downward, without touching each other .
- Ensure cycles achieve an A0 value of at least 3000 (per ISO 15883-1) .
- Remove batteries before automated cleaning .
1. Final Rinse (after chemical disinfection): Rinse the handle thoroughly with sterile or demineralized water to remove all chemical residues .
2. Complete Drying: Air-dry completely on a clean, lint-free surface . Ensure the battery compartment and all crevices are absolutely dry before proceeding.
3. Inspection and Functional Testing:
- Visually inspect for any damage, corrosion, or residual soil .
- Insert fresh batteries and attach a clean blade to verify proper light function . A bright, steady light confirms electrical integrity.
- For video handles, test the display and all electronic functions.
4. Storage: Store the fully assembled, tested laryngoscope in a clean, dry, protected storage cabinet or drawer, ready for immediate use . Proper storage prevents environmental recontamination.
Video laryngoscope handles contain sophisticated electronics and require extra precautions :
1. Strict IFU Adherence: Their reprocessing protocols are highly specific. Never assume immersion is permitted.
2. Wipe-Down Only: Most require meticulous wiping with approved disinfectant wipes. For example, the McGrath Mac Video Laryngoscope in NHS Scotland uses Clinell surface disinfectant wipes (green wipes) for cleaning and low-level disinfection of the handle, blade, and battery compartment . This change was implemented based on a device-specific risk assessment.
3. Protect Electronic Ports: Avoid getting moisture into charging ports, vents, or screen edges.
4. Separate Component Processing: Often, the video blade (containing the camera) is detached and reprocessed separately, while the handle (containing electronics) is only wiped .
5. Battery Management: Follow specific instructions for battery removal or charging during cleaning cycles.
- Not Removing Batteries: This is the most common error, leading to corrosion, device failure, and inadequate disinfection .
- Using Abrasive Materials: Steel wool, scouring pads, or stiff brushes can scratch the handle finish, creating niches where bacteria can hide .
- Incomplete Drying: Storing a damp handle promotes microbial growth and battery corrosion .
- Using Incompatible Chemicals: Alcohol can damage rubber seals and plastics; bleach can corrode metal . Always use manufacturer-approved agents.
- Neglecting the Battery Compartment: This critical hidden surface is often overlooked but must be cleaned and dried thoroughly .
- Assuming All Handles Are Autoclavable: Most standard handles are NOT autoclavable; verify with IFU .
To simplify reprocessing and guarantee infection control, many institutions adopt complementary strategies:
Disposable Laryngoscope Systems: Entirely single-use laryngoscope blade and handle systems eliminate reprocessing entirely. The device is used once and discarded, providing guaranteed sterility for each procedure .
Disposable Plastic Sheath/Covers: A sterile, disposable plastic sleeve is placed over a cleaned laryngoscope handle before each use . This provides a physical barrier—only the sheath contacts the patient and clinician. The handle requires only low-level disinfection between patients, and the sheath must be changed for every patient. This approach significantly reduces reprocessing burden while maintaining infection control.
Cleaning a laryngoscope handle is a non-negotiable, meticulously proceduralized task that sits at the intersection of clinical efficacy and patient safety. It is a multi-step process beginning with immediate point-of-care decontamination and proceeding through meticulous manual cleaning, appropriate high-level disinfection or sterilization, and thorough drying and functional testing. The cornerstone of this process is unwavering adherence to the device-specific Manufacturer's Instructions for Use.
The evidence is clear: inadequately processed laryngoscope handles can transmit infections to patients . Both the laryngoscope blade and handle must be treated as semi-critical items and processed accordingly . Given the complexities and inherent risks of manual reprocessing, the trend towards single-use laryngoscope systems or the use of disposable handle sheaths presents a compelling solution, effectively outsourcing the reprocessing burden to the manufacturer and providing the highest assurance against cross-contamination. Whether maintaining reusable equipment or utilizing disposable barriers, a rigorous, consistent protocol for laryngoscope handle hygiene is an essential investment in preventing healthcare-associated infections and ensuring that this vital airway tool is always safe and ready for its next life-saving use.

No, alcohol swabs are insufficient for proper disinfection of a laryngoscope handle . While alcohol is effective against many pathogens, it is not a high-level disinfectant for all viruses and spores. More importantly, alcohol can degrade rubber seals and plastic components over time. You must use an EPA-registered hospital-grade disinfectant wipe or solution approved by the laryngoscope manufacturer, following the required contact time specified in the instructions.
Batteries should be changed before every use or at the start of each clinical shift . A functional check with a new blade should always be performed. Never use a laryngoscope with weak or old batteries, as a dim light compromises visualization and patient safety. Remove batteries for storage to prevent leakage and corrosion.
It is generally recommended to store them separately . Storing with the blade attached can place stress on the locking mechanism and potentially dull the blade. Furthermore, separate storage in a clean, organized tray or cabinet allows for easy visual inspection and access. The handle should be fully assembled (with batteries and a clean blade) only when prepared for immediate use in a procedure.
Immediately remove it from clinical service . A damaged laryngoscope handle is a patient and staff safety hazard. It can fail during intubation, harbor pathogens in cracks, or have electrical faults. Tag it clearly as "DEFECTIVE" and follow your facility's protocol for medical device repair or disposal. Do not attempt to use it.
The primary advantage is simplified infection control and workflow efficiency . The sterile sheath creates a physical barrier. After use, only the sheath is contaminated and is discarded. The underlying laryngoscope handle requires only a low-level wipe down between patients, not full high-level disinfection. This reduces reprocessing time, eliminates risks associated with incomplete cleaning, and extends the functional life of the handle by minimizing exposure to harsh chemicals.
[1] https://www.unicornendoscope.com/how-to-clean-laryngoscope-handle.html
[2] https://www.heine.com//en_AU/service-support/resources/faq/product-faq/faq/33323-heine-standard-fo-4-led-nt-laryngoskopgriff
[3] https://www.rightdecisions.scot.nhs.uk/sjh-emergency-medicine/handbook/equipment/mcgrath-mac-video-laryngoscope
[4] https://e-safe-anaesthesia.org/sessions/13_01/d/ELFH_Session/1715/tab_2053.html
[5] https://www.heine.com/en/service-support/resources/faq/product-faq
[6] https://www.unicornendoscope.com/how-to-clean-laryngoscope-after-use.html
[7] https://pesquisa.bvsalud.org/portal/resource/p1/mdl-31246299
[8] https://manualzz.com/manual/Welch%2520Allyn/71030
[9] https://manualzz.com/doc/10254787/welch-allyn-60813--60814--60815-fiber-optic-laryngoscope-...