Views: 222 Author: Lake Publish Time: 2026-02-12 Origin: Site








Content Menu
● The Critical Importance of Proper Laryngoscope Blade Cleaning
● Pre-Cleaning at Point of Use: The First Line of Defense
● Step-by-Step Manual Cleaning Protocol
>> Phase 1: Preparation in the Decontamination Area
>> Phase 2: Immersion, Brushing, and Detailed Cleaning
>> Phase 3: Rinsing, Drying, and Inspection
● Automated Cleaning (Washer-Disinfector)
● Post-Cleaning: Packaging and Sterilization
● Common Errors and Best Practices
● The Growing Role of Single-Use Laryngoscopes
● Frequently Asked Questions (FAQs)
>> 1. Can I clean the laryngoscope handle in the same way as the blade?
>> 2. What is the best type of brush to use for cleaning?
>> 3. Why is the hinge area so important to clean?
>> 4. How do I know if the blade is clean enough for sterilization?
>> 5. Is it safe to use an ultrasonic cleaner for laryngoscope blades?
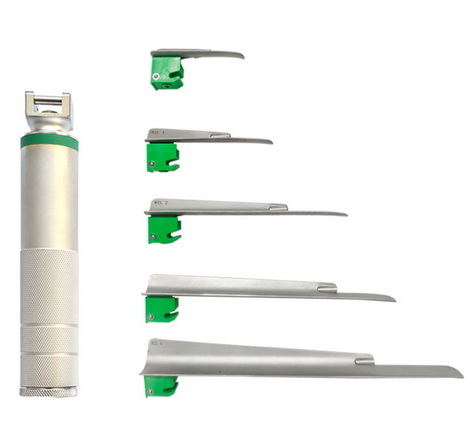
In the critical field of airway management, the laryngoscope is an indispensable tool for visualizing the glottis and facilitating endotracheal intubation. Its reliability and safety are paramount. While single-use devices are growing in popularity, the reusable metal laryngoscope blade remains a staple in many healthcare settings worldwide due to its durability. However, this reusability hinges entirely on one non-negotiable process: meticulous cleaning and sterilization. A contaminated laryngoscope blade is not just a defective tool; it is a vector for potentially fatal healthcare-associated infections (HAIs). This article provides a comprehensive, step-by-step guide on how to properly clean a laryngoscope blade, adhering to the highest standards of infection prevention and control (IPC). As a company specializing in medical visualization and the manufacturing of precision devices, we understand that the clarity of the view depends on the cleanliness of the tool, whether it's a complex endoscope or a fundamental laryngoscope.
The laryngoscope blade is classified as a semi-critical medical device because it contacts mucous membranes (the oropharynx). According to the Spaulding classification and guidelines from global health authorities, it must undergo at least high-level disinfection, but sterilization is the gold standard. Cleaning is the essential, non-skippable first step in this process. Its purpose is physical, not microbiological: to remove all organic material (blood, saliva, secretions), soil, and visible debris. This is crucial because:
1. Organic Matter Protects Pathogens: Residual bioburden can shield microorganisms from the lethal effects of subsequent disinfectants or sterilants (like steam in an autoclave), leading to reprocessing failure.
2. Prevents Biofilm Formation: Inadequate cleaning allows proteins to adhere to the blade surface, creating a tenacious biofilm that harbors bacteria and is extremely resistant to eradication.
3. Ensures Effective Sterilization: Steam or chemical sterilants cannot penetrate layers of dried blood or mucus. A physically clean surface is an absolute prerequisite for effective sterilization.
A failure in cleaning can directly lead to patient harm, including pneumonia, sepsis, and the transmission of pathogens like MRSA or C. difficile.
The reprocessing cycle begins the moment the laryngoscope is removed from the patient's airway.
1. Immediate Wiping: At the bedside or in the procedure room, the blade should be gently wiped with a disinfectant cloth or gauze moistened with an appropriate cleaner to remove gross contamination. This prevents organic material from drying and hardening.
2. Safe Disassembly: Carefully separate the laryngoscope blade from the handle. The handle, which contains electrical components and batteries, must NEVER be immersed in liquid or autoclaved. Handle reprocessing typically involves external wiping only.
3. Safe Transport: Place the contaminated blade in a designated, leak-proof, labeled container (often a basin or rigid container) for transport to the Central Sterile Supply Department (CSSD) or dedicated decontamination area. This prevents environmental contamination during transit.
Manual cleaning remains the cornerstone of effective decontamination, especially for devices with hinges and crevices where automated washers may not reach.
1. Personal Protective Equipment (PPE): The technician must don appropriate PPE: fluid-resistant gown, medical gloves, face shield or mask with goggles.
2. Disassembly: Fully disassemble the laryngoscope blade according to the manufacturer's Instructions for Use (IFU). This almost always involves removing the light source component—either unscrewing a bulb or detaching a fiberoptic light carrier from the blade. *The IFU is the law for device reprocessing.*
3. Initial Inspection: Visually inspect for visible damage, cracks, or deep pitting that could compromise the blade or trap debris.
1. Prepare Solution: Fill a sink or basin with a fresh, properly diluted enzymatic detergent solution. Use lukewarm water (typically below 45°C/113°F) to prevent protein coagulation.
2. Soak: Completely submerge the blade and all disassembled parts. Allow to soak for the time specified by the detergent manufacturer (usually 5-10 minutes) to loosen debris.
3. Meticulous Brushing: Using a soft-bristled, dedicated brush (often a small brush designed for instrument channels), scrub every surface of the laryngoscope blade:
- Scrub the entire spatula (curved or straight portion) thoroughly.
- Pay extreme attention to the hinge mechanism. This is the highest-risk area for biofilm formation. Use the brush tip to scrub inside the knuckle of the hinge.
- Clean the area where the light source attaches, including threads or connectors.
- Brush the locking mechanism (the part that engages with the handle) and any serrations.
- Follow a consistent pattern (e.g., from cleanest to dirtiest area) to ensure no surface is missed.
4. Channel Cleaning: If the blade design incorporates a lumen (e.g., for a fiberoptic bundle), use an appropriately sized lumen brush to clean the internal channel.
1. Thorough Rinsing: After brushing, rinse the blade and all components thoroughly under running water. It is best practice to perform a final rinse with demineralized or distilled water to prevent spotting or mineral deposits from tap water.
2. Detailed Inspection: Under good lighting, visually inspect the cleaned blade. Use magnification if available. Verify that all visible soil, blood, and detergent residue have been removed. Pay special attention to the hinge and crevices. If any debris remains, repeat the brushing and rinsing steps.
3. Drying: Manually dry the blade and all parts completely using a clean, low-lint, disposable cloth. Absolute dryness is critical before packaging for sterilization, as residual moisture can cause "wet packs" in an autoclave, which are considered non-sterile.

Many facilities use automated washer-disinfectors to improve consistency and reduce staff exposure to contaminants.
- Process: The disassembled blade is placed on a dedicated rack to ensure all surfaces are exposed. The machine cycles through phases: flush, wash with enzymatic detergent, rinse, thermal or chemical disinfection, and final drying.
- Limitation: While effective for overall cleaning, automated systems may not provide the direct mechanical action needed for the tight confines of a laryngoscope hinge. Therefore, a preliminary manual brush-cleaning of the hinge is often recommended even when using an automated system.
Once cleaned, dried, and inspected, the blade moves to the preparation and sterilization stage.
1. Functional Check: Ensure the hinge moves smoothly and the blade is not damaged.
2. Packaging: Place the blade in an FDA-cleared sterilization pouch or wrap. Ensure proper sealing and include an internal chemical indicator.
3. Sterilization: The packaged blade must be sterilized, typically using steam sterilization (autoclaving). A common validated cycle for metal instruments is 134°C (273°F) for a minimum of 3 minutes in a pre-vacuum sterilizer. The cycle must be validated for the specific device and pack configuration.
4. Storage and Handling: After sterilization and adequate cooling, the pack is stored in a clean, dry area. Sterility is considered event-related (dependent on package integrity) rather than time-related.
- ERROR: Not fully disassembling the laryngoscope blade.
- BEST PRACTICE: Always separate the light component; follow the IFU meticulously.
- ERROR: Using abrasive pads or wire brushes.
- BEST PRACTICE: Use only soft, non-abrasive brushes to avoid scratching the surface, which can harbor microbes.
- ERROR: Inadequate rinsing, leaving enzymatic or chemical residues.
- BEST PRACTICE: Perform a thorough, final rinse with appropriate water quality.
- ERROR: Packaging a wet blade for sterilization.
- BEST PRACTICE: Confirm the blade is completely dry before sealing the sterilization pouch.
The complexity and risk inherent in the multi-step reprocessing of reusable laryngoscope blades have driven significant innovation. Many leading medical device companies now offer single-use, disposable laryngoscope options, particularly in the video laryngoscope segment. These devices:
- Eliminate Reprocessing Risk: No cleaning, disinfection, or sterilization is required, removing the potential for human error or equipment failure.
- Guarantee Sterility: Each device is factory-sterilized (e.g., by ethylene oxide or gamma radiation) and used once.
- Simplify Logistics: Eliminate the need for CSSD resources, cleaning chemicals, and autoclave capacity.
The choice between reusable and disposable often involves a Total Cost of Ownership (TCO) analysis, weighing the per-unit cost of a disposable device against the cumulative, often hidden, costs of reprocessing a reusable one (labor, utilities, detergent, repair, and capital equipment depreciation).
Cleaning a reusable laryngoscope blade is a meticulous, protocol-driven science that forms the absolute foundation of safe airway management. It requires diligence, proper training, and unwavering attention to detail at every step—from point-of-use wiping to final sterile storage. While this practice is well-established, it carries inherent risks related to human variability and process complexity. This reality underscores the value proposition of modern single-use laryngoscope systems, which offer a definitive solution to these reprocessing challenges. Whether a healthcare facility employs a rigorous reusable protocol or adopts a disposable model, the ultimate goal is unequivocal: to ensure that every patient is intubated with a device that is not only functionally perfect but also microbiologically safe. In the high-stakes environment of airway management, there is no compromise for cleanliness.
Contact us to get more information!

Absolutely not. The laryngoscope handle contains batteries and electronics. It must never be submerged, sonicated, or autoclaved. Cleaning involves wiping the external surfaces with a hospital-grade disinfectant wipe, following the manufacturer's IFU. Always disconnect the blade from the handle immediately after use for separate processing.
Use a soft-bristled, dedicated instrument brush. Brushes should be single-use and disposable, or if reusable, they themselves must be cleaned and high-level disinfected or sterilized after each use to prevent cross-contamination. Avoid stiff or abrasive brushes that can scratch the metal.
The hinge is a complex mechanical joint with tight tolerances and crevices. It is highly prone to trapping blood, saliva, and tissue. If not meticulously cleaned, this area becomes a primary site for biofilm formation, shielding pathogens from disinfectants and leading to reprocessing failure and infection risk.
Perform a visual and tactile inspection under good light. The blade should be visibly free of all soil, streaks, and residue. It should feel smooth and look shiny. Magnification can help. If any discoloration or debris is visible in the hinge or other areas, it must be re-cleaned. "Clean to the naked eye" is the minimum standard.
Ultrasonic cleaners can be effective for metal instruments, but caution is required. You must consult the laryngoscope manufacturer's IFU to confirm compatibility. Ultrasonic cavitation can damage certain materials or delicate components (like some fiberoptic connections). If approved, the blade must still be pre-cleaned of gross debris and the ultrasonic solution must be changed frequently.
[1] https://www.cdc.gov/infectioncontrol/guidelines/disinfection/index.html
[2] https://www.fda.gov/medical-devices/reprocessing-reusable-medical-devices/instructions-use-medical-device-products
[3] https://www.apsf.org/article/laryngoscope-handle-clearing-the-air-on-cleaning-and-sterilization/
[4] https://www.aorn.org/guidelines/clinical-resources/tool-kits/guideline-implementation-tool-kits
[5] https://www.iso.org/standard/73339.html
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3771140/
[7] https://www.astm.org/f3407-20.html