Views: 222 Author: Lake Publish Time: 2025-12-27 Origin: Site








Content Menu
● Sterilization vs. Disinfection: A Critical Distinction
● Foundational Pre-Steps: Cleaning is Non-Negotiable
● Compatible Sterilization Methods for Laryngoscopes
>> 1. Low-Temperature Sterilization (The Most Common Route for Full Sterilization)
>> 2. Steam Sterilization (Autoclaving)
● The Special Case of Video Laryngoscopes
● Process Flow: From Dirty to Sterile
● The Unassailable Role of Manufacturer's Instructions for Use (IFU)
● The Ultimate Guarantee: Single-Use Laryngoscopes
● Frequently Asked Questions (FAQ)
>> 1. Can I autoclave (steam sterilize) my standard metal laryngoscope handle and blade?
>> 2. How do I know if my laryngoscope has been properly sterilized?
>> 4. What is the most critical mistake made during laryngoscope reprocessing?
>> 5. Are single-use laryngoscopes environmentally sustainable?
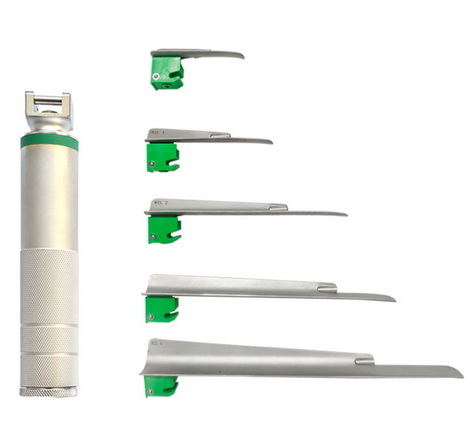
The laryngoscope is a critical tool for securing a patient's airway, a procedure where failure is not an option. However, its intimate contact with the mucous membranes of the oropharynx necessitates the highest standard of reprocessing to prevent iatrogenic infection. While "disinfection" is commonly discussed, the gold standard for patient safety is sterilization. Sterilization is a validated process that destroys all forms of microbial life, including bacterial spores, offering an absolute level of assurance that disinfection cannot guarantee. The question of how to properly sterilize a laryngoscope is therefore central to modern infection control protocols in anesthesia, emergency medicine, and critical care. This comprehensive guide details the principles, methods, and rigorous steps required to achieve sterilization of laryngoscope equipment, differentiating between reusable and disposable systems, and emphasizing the non-negotiable role of manufacturer instructions.

Understanding the goal is paramount. Disinfection eliminates most pathogenic microorganisms on inanimate objects but may not kill bacterial spores. Sterilization eliminates all microbial life. According to the Spaulding classification, a laryngoscope blade is a *semi-critical item* (contacting mucous membranes). The minimum standard is high-level disinfection (HLD). However, leading guidelines from organizations like the Centers for Disease Control and Prevention (CDC) and the Association of periOperative Registered Nurses (AORN) strongly advocate for sterilization when possible, as it provides the highest margin of safety given the device's use in a non-sterile but sensitive body cavity.
Sterilization will fail if the device is not impeccably clean. Organic debris (blood, saliva, protein) can shield microorganisms from the sterilizing agent.
1. Immediate Point-of-Use Treatment: After use, wipe the laryngoscope blade and contaminated parts of the handle with a disinfectant towel to remove gross soil before it dries.
2. Disassembly and Transportation: Remove the blade from the handle. For reusable blades, detach the light bulb if designed for removal. Place all contaminated components in a designated, labeled, leak-proof container for transport to the Central Sterile Supply Department (CSSD) or reprocessing area.
3. Meticulous Manual Cleaning:
- Wear PPE: Gloves, gown, and eye protection.
- Disassemble Completely: Remove batteries from the handle. Take apart all removable components as per the laryngoscope manufacturer's Instructions for Use (IFU).
- Wash: Immerse components (if immersible) in a basin of warm water and an enzymatic detergent. Using soft brushes, thoroughly scrub all surfaces of the laryngoscope blade—crevices, serrations, the light bulb housing, and the locking mechanism. Clean the handle's electrical contacts with a cotton swab.
- Rinse: Rinse all parts thoroughly under running water to remove all detergent residue.
- Dry: Pat dry meticulously with a lint-free cloth. Residual moisture can interfere with certain sterilization methods (e.g., steam).
Not all laryngoscope components can withstand all sterilization methods. The choice is dictated entirely by the device's material composition and the manufacturer's IFU.
Since most laryngoscope handles contain heat-sensitive electronics, plastics, or rubber seals, low-temperature methods are essential.
- Hydrogen Peroxide Gas Plasma (e.g., STERRAD®):
- Process: Components are placed in a chamber where hydrogen peroxide vapor is diffused and then excited into a plasma state by radiofrequency energy, generating free radicals that kill microbes.
- Advantages: Fast cycle time (≈30-75 mins), leaves no toxic residue, safe for most heat- and moisture-sensitive materials.
- Suitability for Laryngoscope: Excellent for metal blades and many plastic/composite handles if validated by the IFU. The device must be completely dry and properly packaged.
- Ethylene Oxide (EtO) Gas:
- Process: A chemical gas that penetrates packaging to kill microbes. Requires a long cycle time (several hours) plus a lengthy aeration period to remove gas residue.
- Advantages: Highly effective penetrative sterilization for complex devices.
- Suitability for Laryngoscope: An effective but less commonly used option due to long turnaround times and environmental/health concerns. Only if explicitly stated in the IFU.
- Liquid Chemical Sterilant Processing (e.g., Extended Soak in Glutaraldehyde):
- Process: Immersion for an extended period (often 6-12 hours) in a concentrated chemical sterilant.
- Disadvantages: Lengthy process, requires perfect rinsing with sterile water to prevent toxic tissue irritation, chemical exposure risks to staff.
- Suitability: Generally considered a less desirable method due to operational and safety challenges, but may be specified in some IFUs.
- Process: Uses saturated steam under pressure at high temperatures (e.g., 121°C/250°F or 134°C/273°F).
- Suitability for Laryngoscope: Most modern laryngoscope handles and blades with plastic, rubber, or fiberoptic components are NOT autoclavable. High heat and moisture will destroy electronics, cause delamination, warp plastics, and crack lenses. Only specific, all-metal, solid-handle laryngoscopes explicitly labeled as "autoclavable" can undergo this process. Always check the IFU.
Modern video laryngoscope systems present a layered sterilization challenge.
1. Disposable Video Blades: The optimal solution. The single-use blade, containing the camera and LEDs, is discarded after use. This removes the most contaminated and difficult-to-clean component from the reprocessing cycle entirely.
2. Reusable Video Blades: Must be sterilized according to a very specific IFU, which almost always dictates a low-temperature method (like hydrogen peroxide gas plasma). They are typically not immersible and require careful cleaning of the camera lens prior to sterilization.
3. Video Handles/Processors: These complex electronic units are never sterilized in a traditional sense. Their processing is limited to:
- External Disinfection: Thorough wiping with an EPA-registered disinfectant wipe approved for electronics.
- Barrier Protection: The use of a single-use, sterile plastic sleeve or sheath that covers the handle during the procedure, creating a physical barrier between the patient/operator and the handle.
- UV-C Light Chambers: Some systems incorporate a charging dock that also exposes the handle to ultraviolet-C light for surface disinfection.
A standardized workflow is crucial:
1. Decontamination Area: Cleaning and disassembly occur here.
2. Packaging: Clean, dry laryngoscope components are wrapped in sterilization-specific packaging (e.g., peel pouches, sterilization wraps). Chemical indicators are placed inside the pack.
3. Loading & Sterilization Cycle: Packages are loaded into the sterilizer (e.g., STERRAD chamber) without overcrowding. The appropriate cycle is selected and run.
4. Monitoring & Release: Sterilization is verified using a combination of:
- Physical Monitors: Time, temperature, pressure.
- Chemical Indicators: Strips or tape on the package that change color when sterilization parameters are met.
- Biological Indicators (BIs): The gold standard. Spore tests (e.g., *Geobacillus stearothermophilus*) are run weekly (or per protocol) to confirm the sterilizer's lethality.
A load is only released for patient use after all monitors indicate success.
5. Storage: Sterile packages are stored in a clean, dry, designated area with controlled access. Integrity of the packaging is paramount; torn or wet packages are considered non-sterile.
The IFU is the legal and technical document that defines the only validated methods for cleaning and sterilizing a specific laryngoscope model. Deviating from the IFU can:
- Void the device warranty.
- Cause irreparable damage to the laryngoscope.
- Invalidate the sterilization process, leading to non-sterile devices being used on patients.
- Expose the healthcare facility to liability.
Given the complexities, costs, and risks associated with reprocessing reusable laryngoscope equipment, single-use, disposable laryngoscopes have become the standard of care for infection prevention in many institutions. These devices are:
- Terminally Sterilized by the manufacturer (typically via gamma irradiation or EtO).
- Used once and then discarded, eliminating any risk of cross-contamination from prior use or reprocessing errors.
- Consistently performant, with each unit offering a new, sharp blade and a fresh battery.
Sterilizing a laryngoscope is a sophisticated, multi-disciplinary process that extends far beyond simple cleaning. It is a quality-assured chain of events that begins with impeccable manual cleaning, proceeds through validated packaging, and culminates in a monitored low-temperature sterilization cycle—all meticulously guided by the manufacturer's IFU. For the heat-sensitive electronics in modern handles, especially video laryngoscope systems, achieving true sterilization of all components is often impractical, necessitating a hybrid approach of handle disinfection/barrier use with blade sterilization or disposal.
The significant operational burden and inherent risk of human error in this chain have powerfully driven the adoption of single-use laryngoscope systems. These devices represent the most straightforward and reliable method to ensure absolute sterility for each patient encounter. Whether an institution chooses to manage the complex lifecycle of reusable equipment or opts for the certainty of disposables, the ultimate objective remains the same: to ensure that every laryngoscope introduced into a patient's airway presents zero risk of infection, allowing clinicians to focus solely on the life-saving task of securing the airway.

Only if the manufacturer's Instructions for Use explicitly state the device is "autoclavable." Most contemporary laryngoscope handles, even metal ones, contain rubber O-rings, plastic light guides, or insulated wires that will be destroyed by the high heat and moisture of an autoclave. Assuming a device is autoclavable without verification is a common and costly error that leads to equipment destruction.
Reliance on a multi-parameter process release is key. Do not rely on a single indicator. Proper sterilization is confirmed by: 1) Physical monitors confirming the cycle completed correctly, 2) Chemical indicators on the outside (and ideally inside) the packaging showing the correct color change, and 3) A successful weekly biological indicator (spore test) for the specific sterilizer being used. The package should be intact, dry, and within its documented expiry period.
While chemical immersion for an extended time (e.g., 10-12 hours) can be a sterilizing process, it is fraught with risk. It requires perfect rinsing with sterile water to remove toxic residues that can cause severe chemical pharyngitis or pneumonitis in patients. It also poses significant occupational health risks to staff from vapor exposure. It is a less reliable and more hazardous method compared to automated low-temperature gas systems and is not recommended as a primary method unless no other option exists per the IFU.
The most critical, and unfortunately common, mistake is inadequate cleaning prior to sterilization. If organic soil (blood, protein) is not completely removed, it can form a barrier that prevents the sterilizing agent (gas plasma, steam, EtO) from contacting and killing all microorganisms on the laryngoscope surface. Sterilization is not a substitute for cleaning; it is the final step that depends entirely on perfect cleaning.
This is a valid concern. While they generate medical waste, a comprehensive life-cycle analysis often reveals a complex picture. Reusable laryngoscope systems have a significant environmental footprint from the constant use of water, energy, chemicals, and packaging for reprocessing, as well as the eventual disposal of damaged parts. The sustainability choice depends on local waste management infrastructure, reprocessing practices, and device design. Manufacturers are increasingly addressing this with responsibly sourced materials and take-back programs for certain components.
[1] https://www.cdc.gov/infectioncontrol/guidelines/disinfection/index.html
[2] https://www.fda.gov/medical-devices/reprocessing-reusable-medical-devices
[3] https://www.aorn.org/guidelines/clinical-resources/tool-kits/processing-of-laryngoscopes