Views: 222 Author: Lake Publish Time: 2025-12-03 Origin: Site








Content Menu
● Introduction: Illuminating the Pathway to a Pivotal Invention
● Pre-Laryngoscope Era: The Challenge of the Unseen Larynx
● The First Direct Laryngoscope: Horace Green and the "American Method"
● The Father of Direct Laryngoscopy: Johann Nepomuk Czermak and the Convergence of Light and Optics
● The "Invention" Milestone: The 1895 Laryngoscope of Alfred Kirstein
● Refinement for Anesthesia: The Contributions of Chevalier Jackson and Robert Reynolds Macintosh
● The Modern Evolution: From Fiber Optics to Video Laryngoscopes
● Conclusion: A Legacy of Illumination and Innovation
● Frequently Asked Questions (FAQ)
>> 1. Who is officially credited with inventing the first direct laryngoscope?
>> 2. Did Manuel García invent the laryngoscope?
>> 3. What was the key technological advancement that made Kirstein's laryngoscope possible?
>> 4. How did the Macintosh blade change the use of the laryngoscope?
The laryngoscope, a seemingly simple instrument composed of a handle and a blade, stands as one of the most transformative devices in the history of medicine. Its invention fundamentally changed the practices of anesthesiology, otolaryngology, and emergency medicine by providing a direct, illuminated view of the larynx—a gateway to the lungs that was once shrouded in darkness and guesswork. But pinpointing a single date for the invention of the laryngoscope is a journey through medical history, marked by incremental innovations, brilliant insights, and the convergence of several key technological advancements. This article traces that journey, exploring the key figures and milestones that led to the modern laryngoscope, an instrument that remains indispensable in medical visualization and airway management today.
For a company like ours, deeply embedded in the field of medical visualization through devices like video laryngoscopes and flexible laryngoscopes, understanding this historical foundation is crucial. It connects our work to a legacy of innovation aimed at solving the perennial clinical challenge of securing a patient's airway. The story of the laryngoscope is not just about a tool; it's about the evolution of a concept—from indirect mirror-based examinations to direct visualization, and now to enhanced digital imaging.

Before the laryngoscope, the larynx was a "hidden organ." Physicians had no reliable means to examine it in living patients. Diagnoses of laryngeal conditions, such as tumors or infections, were largely based on external symptoms, voice changes, and indirect evidence, often leading to late intervention and poor outcomes. In surgery and emergency care, managing an obstructed airway or facilitating anesthesia was a perilous, blind procedure. Tracheotomy was a risky, last-resort operation.
The first significant breakthrough came with the development of indirect laryngoscopy. In 1854, a Spanish singing teacher named Manuel García, often credited as the father of indirect laryngoscopy, used a dental mirror and a second hand mirror to reflect sunlight onto his own vocal cords. By observing the reflected image, he became the first person to view a living larynx in action. While García's technique was a monumental scientific discovery, it was a diagnostic tool for studying physiology, not a practical device for therapeutic intervention or airway management in patients. It required patient cooperation, good lighting, and considerable skill, limiting its use in surgical or emergency settings.
The leap from indirect viewing to direct examination is often attributed to an American physician, Dr. Horace Green. In the 1840s, Green developed a technique for treating laryngeal obstructions in children. He used a bent tongue spatula to depress the tongue and, with the aid of sunlight, attempted to view and treat the larynx directly. He even reported removing a laryngeal polyp using this method in 1852. His 1852 textbook detailed these procedures.
However, Green's method was controversial, painful, and dangerous without proper anesthesia or a reliable light source. It was known as the "American method" but was not widely adopted or standardized. His instrument was more of a specialized spatula than a true laryngoscope system. While Green demonstrated the possibility of direct laryngeal intervention, his work lacked the critical components that would define the modern laryngoscope: a dedicated light source and a designed blade for retraction and visualization.
The pivotal figure who synthesized the key elements was the Austrian-Hungarian physician Johann Nepomuk Czermak. In the late 1850s, Czermak significantly refined the technique of indirect laryngoscopy. Crucially, he replaced sunlight with artificial light—specifically, the light from a lamp—and used a head mirror to concentrate this light into the patient's mouth. This was a revolutionary step, freeing laryngoscopy from dependence on daylight and making examinations more controllable.
Czermak's true genius, however, lay in his experimentation. He began modifying existing tools, including a tool called a *glottiscope*, to attempt direct views. While his primary legacy is in perfecting indirect techniques, his systematic work with mirrors, light, and instrumentation created the essential knowledge base and sparked wider interest in laryngeal visualization. He demonstrated that with adequate illumination, the larynx could be made visible.
The device recognizably called a laryngoscope was invented by a German physician, Dr. Alfred Kirstein, in 1895. Dissatisfied with the limitations of indirect techniques for emergency airway management, Kirstein pioneered a method of "autoscopy" – direct viewing of the larynx. His landmark invention is documented in his 1895 paper, "Autoscopy of the Larynx and Trachea" (*Die Autoskopie der Luftröhre und der Bronchien*).
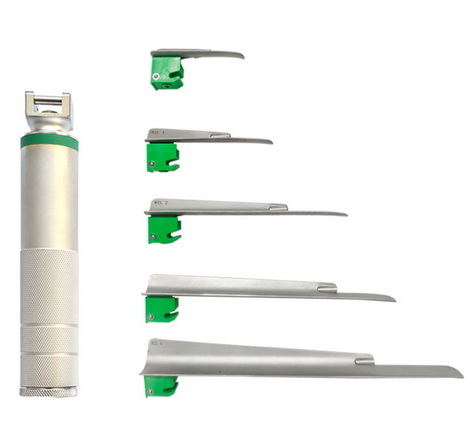
Kirstein's laryngoscope was a purpose-built instrument. It consisted of a straight metal blade, designed to retract the epiglottis and tongue, and a handle. Most importantly, it incorporated an electric light bulb at its distal end, providing direct illumination of the laryngeal inlet. This combination—a dedicated blade for retraction and a built-in distal light source—is the fundamental architecture of the modern direct laryngoscope. Kirstein's invention was intended primarily for diagnostic inspection and foreign body removal, not specifically for endotracheal intubation, but it provided the essential tool that would later be adapted for that purpose.

Following Kirstein, the laryngoscope was refined for broader medical use. American laryngologist Chevalier Jackson standardized and popularized the instrument in the early 20th century. He created a comprehensive set of straight blades, improved lighting, and wrote detailed procedural manuals. His work made direct laryngoscopy a standard ENT procedure.
The adaptation of the laryngoscope for endotracheal intubation, its most common use today, was driven by the needs of anesthesiology. In 1943, British anesthetist Sir Robert Reynolds Macintosh introduced his famous curved blade laryngoscope. Macintosh identified that a curved blade could be used to indirectly lift the epiglottis by placing it in the vallecula (the space between the base of the tongue and the epiglottis), reducing trauma and providing a better view. The "Macintosh blade" became, and remains, the most widely used laryngoscope blade design globally for routine intubation. This innovation solidified the laryngoscope's role as the cornerstone of safe general anesthesia and emergency airway management.
The latter half of the 20th century saw further evolution. The introduction of fiber optic bundles in the 1960s led to the flexible fiberoptic laryngoscope, pioneered by Shigeto Ikeda, which allowed for nasal intubation and examination of awake patients. This was a paradigm shift, enabling intubation in patients with difficult airways without requiring a direct line of sight.
The most significant recent advancement is the video laryngoscope, emerging in the early 2000s. This device incorporates a miniature digital camera at the tip of the blade, transmitting a real-time image to a screen. This provides a magnified, high-resolution view, often with a wider angle than direct line-of-sight, dramatically improving first-pass success rates in difficult airways and enhancing training. As a manufacturer in this space, we see the video laryngoscope as the natural culmination of the historical quest started by García and Kirstein: to obtain the clearest, most reliable view of the larynx possible.
So, when was the laryngoscope invented? The most precise answer points to Alfred Kirstein in 1895, as he created the first integrated instrument with a blade and distal light source designed for direct laryngeal visualization. However, this invention was not a singular event but the climax of a century of progressive ideas—from García's mirrors to Green's direct attempts to Czermak's controlled light. The laryngoscope is a testament to iterative innovation.
From Kirstein's electric bulb to today's high-definition digital sensors, the core mission remains unchanged: to illuminate and visualize the airway for diagnosis and lifesaving intervention. The journey from the 1854 mirror to the modern video laryngoscope encapsulates the history of medical technology itself—each generation building upon the last to improve patient care. For clinicians and manufacturers alike, the story of the laryngoscope serves as a powerful reminder that behind every piece of modern medical equipment lies a rich history of problem-solving, ingenuity, and the relentless pursuit of seeing what was once unseen.
The official credit for inventing the first direct laryngoscope, defined as an instrument with a blade and a distal light source for direct viewing, goes to Dr. Alfred Kirstein, a German physician, in 1895.
No, Manuel García did not invent the laryngoscope. In 1854, he pioneered *indirect laryngoscopy* using mirrors and sunlight to view his own larynx. This was a foundational discovery that proved the larynx could be visualized, but it did not involve the handheld blade-and-handle instrument used for direct examination and intubation.
The key advancement was the integration of a small electric light bulb at the distal end of the blade. Before this, practitioners relied on reflected sunlight or external lamps. A built-in, controllable light source directed into the airway was the critical component that made reliable direct laryngoscopy practicable.
Introduced in 1943 by Robert Macintosh, the curved blade revolutionized the laryngoscope for endotracheal intubation. Instead of lifting the epiglottis directly (as with a straight blade), the Macintosh blade is designed to sit in the vallecula and indirectly lift the epiglottis. This technique is generally less traumatic, provides a consistent view, and made the laryngoscope the primary tool for anesthesiologists worldwide.
A traditional direct laryngoscope requires the operator to align their eye, the blade, and the laryngeal opening in a straight line to see directly through the mouth. A video laryngoscope has a camera at the blade's tip, transmitting the image to a separate screen. This eliminates the need for a direct line of sight, often provides a better view (especially in difficult anatomies), and allows for shared viewing and recording.