







Content Menu
● Fundamental Design and Components
● Clinical Applications and Procedures
● Ureteroscopic Technique and Procedure Steps
● Advantages Over Traditional Surgical Approaches
● Potential Complications and Risk Management
● Maintenance and Sterilization Protocols
● Future Directions and Technological Innovations
>> 1. What is the difference between a rigid and flexible ureteroscope?
>> 2. What conditions typically require ureteroscope procedures?
>> 3. How is a ureteroscope different from a cystoscope?
>> 4. What are the main advantages of ureteroscope procedures?
>> 5. Are there disposable ureteroscope options available?
A ureteroscope represents a sophisticated medical instrument specifically designed for the examination and treatment of conditions within the upper urinary tract, particularly the ureters and kidneys. This specialized endoscope enables urologists to navigate the delicate pathways of the urinary system with remarkable precision, providing both diagnostic capabilities and therapeutic interventions. The modern ureteroscope has revolutionized the field of urology by offering a minimally invasive alternative to traditional open surgical procedures for managing urinary stones, tumors, and other urological conditions. Understanding the ureteroscope requires exploring its technological components, operational mechanisms, clinical applications, and the significant impact it has made on patient care outcomes. As medical technology continues to advance, the ureteroscope has evolved from a simple rigid instrument to sophisticated flexible and digital systems that offer enhanced visualization and therapeutic capabilities for complex urological procedures.

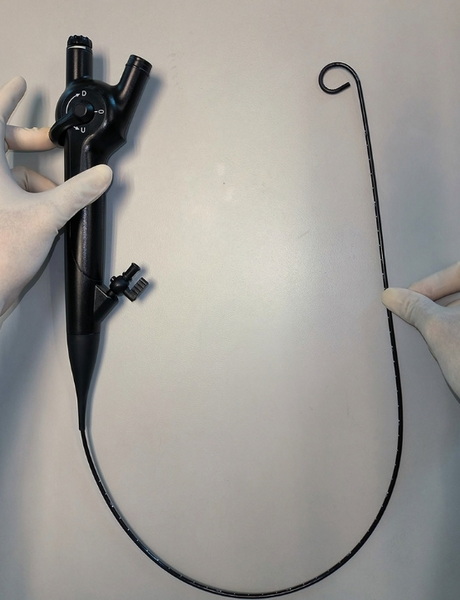
The fundamental design of a ureteroscope incorporates several essential components that work in concert to enable visualization and intervention within the urinary tract. A standard ureteroscope consists of a long, thin shaft that must be narrow enough to navigate the ureter's natural diameter, typically ranging from 2.5 to 3.5 millimeters. The distal tip of the ureteroscope contains the optical system, which may utilize fiber optic bundles or digital camera technology to transmit images from inside the body to the urologist's viewfinder or monitor. This optical component is complemented by a light guide system that illuminates the dark confines of the urinary tract, allowing clear visualization during ureteroscope procedures.
The ureteroscope design also incorporates an irrigation channel that permits the controlled flow of sterile fluid into the urinary tract, serving to distend the ureter for better visualization and flush away blood or debris that might obscure the view. Additionally, the ureteroscope features a working channel through which various specialized instruments can be passed, including laser fibers for stone fragmentation, biopsy forceps for tissue sampling, stone baskets for retrieval, and guidewires for navigation assistance. The proximal end of the ureteroscope contains the eyepiece or video connection, deflection controls for flexible scopes, and ports for irrigation and instrument access. This comprehensive design makes the ureteroscope a versatile tool for both diagnostic and therapeutic urological interventions.
The evolution of ureteroscope technology has produced several distinct types, each with specific characteristics and clinical applications. Rigid ureteroscope models feature a straight, non-bending shaft typically made of metal, providing excellent image quality and a large working channel relative to their diameter. This type of ureteroscope is particularly effective for procedures in the straight portions of the ureter, especially the mid and distal segments, where their lack of flexibility is not a significant limitation. The rigid ureteroscope offers superior irrigation flow and accommodates larger instruments, making it ideal for managing larger stones or performing procedures requiring substantial irrigation.
Flexible ureteroscope designs represent a significant advancement in endourology, featuring a shaft that can be actively deflected in multiple directions to navigate the tortuous anatomy of the upper urinary tract. This type of ureteroscope is essential for accessing the kidney itself, particularly the lower pole calyces which are often challenging to reach with rigid instruments. The modern flexible ureteroscope typically offers deflection capabilities of 270 degrees or more, allowing comprehensive inspection of the entire renal collecting system. A third category, the semi-rigid ureteroscope, combines some characteristics of both rigid and flexible designs, offering limited flexibility while maintaining the image quality and irrigation advantages of rigid scopes. The choice between these ureteroscope types depends on the specific clinical scenario, anatomical considerations, and the urologist's expertise and preference.
The ureteroscope has undergone remarkable technological evolution since its initial development, significantly enhancing its diagnostic and therapeutic capabilities. The transition from fiber optic to digital ureteroscope systems represents one of the most significant advancements in the field. Digital ureteroscope technology utilizes a miniature CMOS or CCD sensor chip at the distal tip of the instrument, capturing high-resolution images directly from within the urinary tract. This digital ureteroscope design provides superior image quality compared to traditional fiber optic systems, with better resolution, color reproduction, and contrast that facilitates the identification of subtle mucosal abnormalities and stone characteristics.
Additional technological enhancements in modern ureteroscope systems include improved deflection mechanisms that offer greater range and precision of movement within the renal anatomy. Some contemporary ureteroscope models feature enhanced irrigation systems that maintain visualization in bloody fields, which is particularly valuable during therapeutic procedures. The development of single-use disposable ureteroscope systems addresses concerns regarding infection control, repair costs, and availability associated with reusable scopes. Furthermore, integration of advanced imaging modalities such as narrow-band imaging with the ureteroscope enables better detection of urothelial carcinomas by highlighting vascular patterns that might be missed with white light alone. These technological improvements continue to expand the diagnostic and therapeutic potential of the ureteroscope in modern urological practice.
The ureteroscope serves as the cornerstone instrument for numerous diagnostic and therapeutic procedures in contemporary urology. The most common application of the ureteroscope is in the management of urinary calculi, particularly ureteral and renal stones that are not amenable to extracorporeal shock wave lithotripsy. During ureteroscope stone procedures, urologists can visualize stones directly, fragment them using laser energy delivered through the scope's working channel, and retrieve the fragments using specialized baskets. This ureteroscope-guided approach has largely replaced open surgical procedures for stone disease, offering significantly reduced patient morbidity, shorter recovery times, and improved stone-free rates for many stone types and locations.
Beyond stone management, the ureteroscope plays a crucial role in the diagnosis and treatment of upper tract urothelial carcinoma. Using the ureteroscope, urologists can directly visualize suspicious lesions, obtain biopsy specimens for pathological evaluation, and administer topical chemotherapeutic agents directly to tumor sites. The ureteroscope also facilitates the management of ureteral strictures through direct visual guidance of balloon dilation or endoscopic incision procedures. Additionally, the ureteroscope is invaluable for diagnosing unexplained hematuria (blood in the urine), identifying sources of bleeding, and evaluating congenital abnormalities of the upper urinary tract. The versatility of the ureteroscope across these diverse clinical scenarios underscores its fundamental importance in modern urological practice.
The successful use of a ureteroscope requires meticulous technique and a systematic approach to ensure both procedural efficacy and patient safety. A standard ureteroscope procedure begins with cystoscopy to examine the bladder and identify the ureteral orifices. The urologist then places a safety guidewire under fluoroscopic guidance up the ureter and into the renal collecting system, providing a secure pathway for ureteroscope advancement. In many cases, the ureteral orifice requires dilation, either with graduated dilators or a balloon dilator, to accommodate the ureteroscope,
particularly when dealing with narrow ureters or impacted stones.
Once access is established, the ureteroscope is carefully advanced over the guidewire or alongside it under direct vision, with continuous irrigation to maintain visualization and distend the ureteral lumen. The urologist systematically examines the ureteral mucosa as the ureteroscope ascends, identifying any pathology, stones, or anatomical variations. Upon reaching the area of interest, the ureteroscope enables targeted intervention, whether stone fragmentation, tumor resection, stricture dilation, or biopsy acquisition. Throughout the procedure, the urologist must maintain awareness of ureteroscope position and orientation to prevent inadvertent injury to the delicate urothelium. The procedure concludes with careful ureteroscope withdrawal while inspecting the mucosa again for any iatrogenic injury or previously missed pathology.
The ureteroscope offers numerous advantages over traditional open surgical approaches for managing upper urinary tract pathology, contributing to its widespread adoption in urological practice. The minimally invasive nature of ureteroscope procedures results in significantly reduced patient morbidity compared to open surgery, with smaller or no external incisions, less postoperative pain, and shorter recovery times. Patients undergoing ureteroscope procedures typically experience shorter hospital stays, with many cases performed on an outpatient basis or requiring only 23-hour observation. This translates to substantial healthcare cost savings and quicker return to normal activities for patients.
From a diagnostic perspective, the ureteroscope provides direct visualization of the upper urinary tract mucosa, offering superior assessment compared to indirect imaging modalities alone. The therapeutic capabilities of the ureteroscope allow for precise, targeted intervention while preserving surrounding healthy tissue, which is particularly important in functional organs like the kidneys. The ureteroscope also enables procedures in patients who are poor candidates for open surgery due to comorbidities, as it generally carries lower anesthetic requirements and physiological stress. Additionally, the ureteroscope can often address pathology in a single setting that might otherwise require multiple procedures with alternative approaches, enhancing treatment efficiency and patient convenience.
While ureteroscope procedures are generally safe, understanding potential complications is essential for optimal patient management. The most common complications associated with ureteroscope use include ureteral injury, which can range from minor mucosal abrasions to more significant perforations. These injuries typically occur during ureteroscope advancement or manipulation, particularly in narrow or tortuous ureters or when navigating past impacted stones. To minimize this risk, urologists employ careful technique, adequate lubrication, and sometimes preoperative stent placement to passively dilate the ureter before the main ureteroscope procedure.
Infection represents another potential complication following ureteroscope procedures, as instrumentation of the urinary tract can introduce bacteria or facilitate systemic absorption of irrigant fluid. Proper sterile technique during ureteroscope use, preoperative urine culture with appropriate antibiotic treatment when indicated, and judicious use of irrigation pressure help mitigate infectious risks. Other potential complications of ureteroscope procedures include bleeding, which is usually self-limited, and ureteral stricture formation as a late complication from mucosal injury. Avulsion of the ureter represents a rare but serious complication that is almost entirely preventable with careful ureteroscope technique and avoidance of excessive force during instrument manipulation or stone extraction.

Proper maintenance and sterilization of reusable ureteroscope systems are crucial for ensuring device longevity, optimal performance, and patient safety. The delicate nature of the ureteroscope, particularly flexible models with complex deflection mechanisms and optical systems, requires specialized handling and cleaning protocols. Immediately after each procedure, the ureteroscope should undergo thorough bedside cleaning to remove organic material and prevent biofilm formation, which can compromise both instrument function and sterilization efficacy.
The formal reprocessing of a ureteroscope typically involves several stages: leak testing to identify any compromise in the instrument's integrity, manual cleaning with enzymatic detergents specifically designed for medical instruments, and high-level disinfection or sterilization using methods compatible with the ureteroscope's materials and electronic components. Increasingly, many institutions are transitioning to single-use disposable ureteroscope systems that eliminate reprocessing concerns entirely, though this approach raises different considerations regarding cost and environmental impact. For reusable ureteroscope systems, proper storage in dedicated containers that protect the delicate shaft and deflection mechanisms is essential for maintaining instrument function between procedures.
The future of ureteroscope technology continues to evolve with several promising innovations on the horizon. Enhanced visualization capabilities represent an active area of development, with research focusing on ureteroscope systems incorporating confocal laser endomicroscopy, optical coherence tomography, and fluorescence imaging to provide microscopic-level tissue characterization during procedures. These advanced ureteroscope technologies could enable real-time pathological assessment without the need for tissue removal, potentially revolutionizing the diagnosis and management of upper tract urothelial carcinoma.
Robotic ureteroscope systems represent another frontier in endourology, offering potential benefits in stability, precision, and ergonomics for the urologist. Early robotic ureteroscope platforms demonstrate feasibility in navigating the complex renal anatomy and maintaining stable positions during therapeutic interventions. Additionally, continued miniaturization of ureteroscope designs may further reduce procedural trauma while maintaining or improving functionality. The integration of artificial intelligence with ureteroscope systems holds promise for automated stone detection, characterization of suspicious lesions, and even procedural guidance. As these technologies mature, the ureteroscope will likely become an even more powerful tool for minimally invasive diagnosis and treatment of upper urinary tract pathology.
The ureteroscope stands as a remarkable achievement in medical technology, fundamentally transforming the management of upper urinary tract disorders. This sophisticated instrument has evolved from a simple diagnostic tool to a comprehensive therapeutic platform that enables urologists to address complex conditions with minimal patient trauma. The continued refinement of ureteroscope design, particularly the development of flexible and digital systems, has expanded the boundaries of endourology, allowing access to virtually the entire upper urinary tract. As technology advances, the ureteroscope continues to incorporate new capabilities that enhance visualization, treatment precision, and procedural efficiency. Despite these technological innovations, the successful application of the ureteroscope remains dependent on the urologist's skill, judgment, and understanding of urinary tract anatomy and pathology. The ongoing evolution of ureteroscope technology promises to further improve patient outcomes while maintaining the minimally invasive approach that has made this instrument indispensable in modern urological practice.
A rigid ureteroscope features a straight, non-bending shaft typically made of metal and is primarily used for procedures in the straight portions of the ureter, offering excellent image quality and a relatively large working channel. In contrast, a flexible ureteroscope has an actively deflectable tip that can navigate the tortuous anatomy of the kidney, particularly the lower pole calyces, making it essential for renal procedures. The choice between rigid and flexible ureteroscope depends on the location of the pathology, with rigid scopes ideal for the mid and distal ureter, while flexible scopes are necessary for accessing the proximal ureter and intrarenal collecting system.
The ureteroscope is commonly used for managing urinary stones, particularly those in the ureter or kidney that haven't passed spontaneously or aren't amenable to extracorporeal shock wave lithotripsy. Additionally, the ureteroscope is essential for diagnosing and treating upper tract urothelial carcinoma, allowing direct visualization, biopsy, and treatment of tumors. Other indications for ureteroscope use include evaluating unexplained hematuria (blood in the urine), managing ureteral strictures through dilation or incision, retrieving foreign bodies, and diagnosing congenital abnormalities of the upper urinary tract.
While both the ureteroscope and cystoscope are endoscopic instruments used in urology, they differ significantly in design and application. The cystoscope is shorter and typically has a larger diameter, designed specifically for examining the bladder and lower urinary tract. In contrast, the ureteroscope is longer, narrower, and often more flexible, engineered to navigate the smaller, tortuous anatomy of the ureters and renal collecting system. The ureteroscope requires greater precision and specialized training to manipulate effectively within the confined spaces of the upper urinary tract compared to the cystoscope.
The ureteroscope offers numerous advantages, primarily its minimally invasive nature which results in reduced patient trauma, less postoperative pain, shorter hospital stays, and quicker recovery compared to open surgical approaches. The ureteroscope provides direct visualization of the upper urinary tract, allowing precise diagnosis and targeted treatment while preserving surrounding healthy tissue. Additionally, ureteroscope procedures typically require only spinal or general anesthesia rather than the more extensive anesthesia needed for open surgery, making them suitable for patients with significant comorbidities who might be poor candidates for traditional surgical approaches.
Yes, single-use disposable ureteroscope systems have become increasingly available and popular in recent years. These disposable ureteroscope options eliminate concerns regarding reprocessing efficacy, cross-contamination between patients, and repair costs associated with reusable scopes. The disposable ureteroscope ensures consistent performance and image quality with each use, as there is no deterioration from repeated sterilization procedures or accumulated wear and tear. While the per-procedure cost may be higher than reusable ureteroscope systems when considering only instrument expense, disposable options may offer economic advantages when factoring in reprocessing costs, repair expenses, and inventory management.
[1] https://www.urologyhealth.org/urology-a-z/u/ureteroscopy
[2] https://www.ncbi.nlm.nih.gov/books/NBK560556/
[3] https://www.auanet.org/education/auauniversity/education-products/course-modules/ureteroscopy
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4708570/
[5] https://www.kidney.org/atoz/content/kidneystones_ureteroscopy
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5819168/
[7] https://www.sciencedirect.com/topics/medicine-and-dentistry/ureteroscopy
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6491193/
[9] https://www.urotoday.com/library-resources/ureteroscopy/1156-ureteroscopy-technique.html